Any healthcare company that builds products or talks with customers ought to have an “Innovation Center”. The idea is to create a physical facility that is part consumer lab, part living laboratory, and part workplace- aimed at designing and delivering the healthcare models of the future. It will be an environment where all organizational and community stakeholders can experience your company’s view of the future of healthcare and be inspired to help create it. An Innovation Center can incorporate the brand promise within a physical setting. An Innovation Center shows true commitment to practice innovation in healthcare. It is time for all healthcare companies embrace the future the way the Mayo Clinic has done for years.
To get started on what I am about to talk about, watch this virtual walk-through of the Mayo Clinic Center for Innovation.
What is an Innovation Center and Why Would You Need One?
The main objectives for an Innovation Center are:
- 1. Designing
- 2. Prototyping
- 3. Collaborating
- 4. Simulating
- 5. Validating
- 6. Envisioning
Lets discus them in some detail.
1. Designing.
Job # 1 of an Innovation Center should be to create (and improve upon) intentional experiences for your customers. You cannot have a good experience without good design. The Customer lab can serve as the place to visualize and practice Design Thinking. Wikipedia defines Design Thinking as “a style of thinking [designed with] the ability to combine empathy for the context of a problem, creativity in the generation of insights and solutions, and rationality to analyze and fit solutions to the context. “
An Innovation Center lets you teach the process and the methods of Design Thinking. These are the tools and techniques that great designers use to generate ideas and solve problems. Your aim should be to create an employee base trained in the arts of creative problem-solving.

2. Prototyping.
Job # 2 of an Innovation Center should be to create faster paths to market for new products and models. One such method to do this is referred to as rapid prototyping and uses the discipline of Minimum Viable Product (MVP). MVP enables designers to validate assumptions about their “product” in two important aspects: its value and the demand for it.
By definition, MVP is the version of a product that gets built through one cycle of a build, measure, and learn loop – as fast as possible. Once the MVP is confirmed (keep in mind it may take a few iterations), other lean methodologies can be employed to build upon it. An Innovation Center allows this rapid prototyping to occur outside the traction of the legacy product and technology build systems at your company. MVP delivered through an Innovation Center enables product developers, system designers, and business analysts to determine whether people want what they are building – in a manner that gauges acceptance and demand – yet preserves capital and time for your company.
3. Collaborating.
Job # 3 of an Innovation Center should be to create a physical place designed to facilitate adult learning and team collaboration. As discussed in the book Where Good Ideas Come From: The Natural History of Innovation, big ideas are a series of smaller ideas coming together to form something that is meaningful to the market. The Innovation Center should be a co-laboratory that brings multi-disciplinary thinkers together on a common problem. Think of it as a modern version of a Library, except you are allowed to talk, experiment, and interact on topics of importance to your customers and your company.
You cannot ask people to collaborate on work if there has been no historical support for collaboration at your company – they simply just do not know how. They remember when they were kids but were programmed out of that model through a progression of educational settings and work scenarios where individual work product was the mode of operation. Asking people to change their work models without giving a realistic means to do so is merely rhetoric. An Innovation Center is designed to force interaction between co-workers. When combined with modern adult learning techniques like teaching collaboration, an Innovation Center can be the breakthrough that your company needs to re-educate its employees on how to work together.
4. Simulating.
Job # 4 of an Innovation Center should be to create a place to simulate customer interactions. Simulation is another great tool for adult education. While classroom learning and computer-based training still have their (small) place in the arsenal of training tools, nothing substitutes simulating a real life scenario to embed the training into the mind, and actions, of the trainee.
If your current training facilities do not invoke/inspire interest and a spirit of learning about how the customer feels in response to your customer-facing interactions – consider extending the facilities into an Innovation Center. Use the space as a simulation center to teach how to deliver the best results to a member and video it to review in private.
I had the opportunity to a take tour of the CAMLS — Center For Advanced Medical Learning And Simulation in Tampa, FL. I was highly impressed with this innovation facility and what it will accomplish for the future of medicine and healthcare. You can see some images from my time there in this short video.
5. Validating.
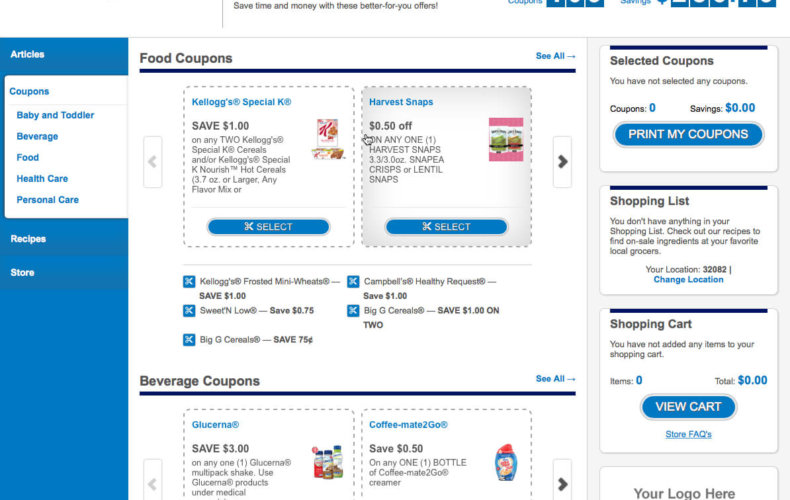
Job # 5 of an Innovation Center should be to create a place to have customers provide feedback on your company’s products and services. Part of the MVP concept mentioned above requires feedback. Healthcare is not like software – it is harder to have Beta users and not create tenuous or even dangerous situations. Proper validation through customer feedback is essential to great product design.
An Innovation Center as a customer lab allows this to happen with the control and confines of your company and reduces the need to pay outside parties to accomplish this oft-repeated task. To be a great consumer company, your company should foster its ability to do firsthand consumer research.
6. Working.
Job # 6 of an Innovation Center should be to your workplace of the future. Unless your company offers workspace like Google (and there are many of these, especially in Austin!) – consider using your space to transform your company’s cube farm into a dynamic workplace. Even if you are doing the best work on Earth, if you are sitting in a cube farm only lit by artificial overhead lighting, chances are you are miserable. Employers are obligated to make great environments for all people to work in, not just the executives. But convincing leaders about what this space should look like is hard to do.
An Innovation Center is supposed to look different – so make it your staging ground for your transforming workplace. Build it with the most modern yet simple furniture. Give it the technology bells and whistles that are fun to use and make people happier when using them. Keep it open and well lit. Provide couches and comfortable chairs to think in. Make it like everybody’s favorite thinking place – Starbuck’s. This will greatly enhance the employee experience and value proposition – and as a result, create a more productive workforce.
7. Envisioning.
Job #7 of an Innovation Center should be to create a fluid understanding of what the future of healthcare might look like. According to Microsoft, their “Microsoft Innovation Centers (MICs ) are state of the art technology facilities for collaboration on innovative research, technology or software solutions, involving a combination of government, academic and industry participants.” Apparently there are now more than 100 Microsoft Innovation Centers worldwide. IBM has several IBM Innovation Centers as well. The concept used at Microsoft’s Innovation Center is “Behind this door lies the future – not a vision of what we want, but a vision of what will be.” Your company should adopt this philosophy as well.
Telling is greatly improved by showing. Teaching a man to fish is how the old adage goes – try putting the pole in his hand near the water, and you are off to the races. Showing removes the need for employees to try and interpret what your leaders are envisioning. Instead, it evokes people to quickly debate on what they see or come up with ideas on how best to implement them. This should be a focus for your company.
Justifying the Cost
In Summary, an Innovation Center can be easily justified as both a capital expenditure and a resource development tool. To compete in a consumer economy, a company needs the capacity to think, react, and dream at the speed of the customer. The natural functioning of business units is contrary to this need. A customer lab opens up the ability for consumer thinking for the whole company, without jeopardizing the current operations.
So the question is not, how can an insurance plan justify an innovation center on an ongoing basis? – but how can they not if they want to become great consumer healthcare companies?
But a word of caution on this idea – companies and the people that work for them change – what is needed today will be old hat tomorrow. If you are going to build your own innovation center – don’t pour it in concrete. Meaning, save room for new ideas and build it modularly so sections that are no longer relevant can be removed.
To your health,
The Team at imagine.GO














 The adjacent image shows a spectrum of how healthcare is managed and paid for in the United States. The area in lighter blue represents the monies paid into the “system” for care, while the darker blue shows the amount “at-risk” by the care providers. The intent is to move away from a fragmented fee-for-service model that only responds to volume, has limited integration across care providers, and treats health in a reactive model. Many label this as “sick-care.”
The adjacent image shows a spectrum of how healthcare is managed and paid for in the United States. The area in lighter blue represents the monies paid into the “system” for care, while the darker blue shows the amount “at-risk” by the care providers. The intent is to move away from a fragmented fee-for-service model that only responds to volume, has limited integration across care providers, and treats health in a reactive model. Many label this as “sick-care.”





